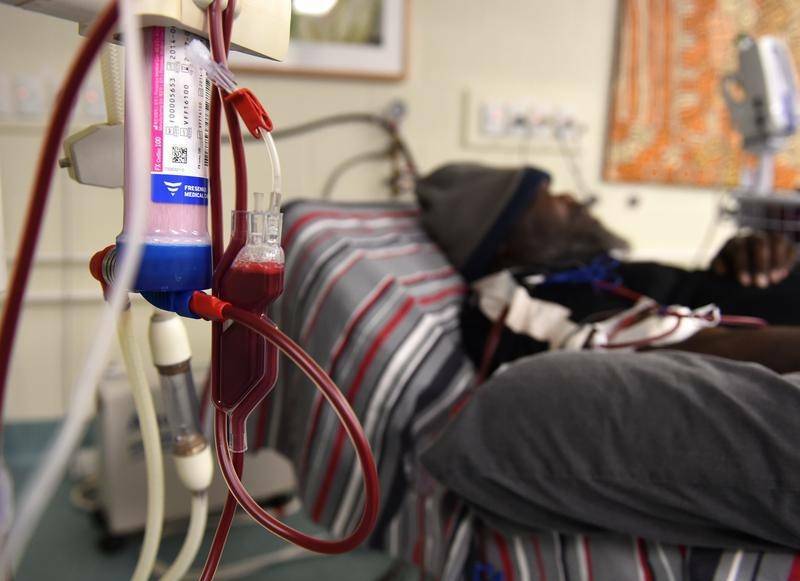
Indigenous people are being encouraged to create their own My Health Record.
Subscribe now for unlimited access.
$0/
(min cost $0)
or signup to continue reading
According to leading health practitioners, My Health Record plays a positive role in improving health outcomes for Indigenous and Torres Strait Islander people.
“Having a My Health Record can be particularly beneficial for Aboriginal and Torres Strait Islander people who may have chronic health conditions, those who move around a lot and those who live in remote areas of Australia,” professor Meredith Makeham, chief medical adviser at the Australian Digital Health Agency said.
“It can save lives in emergency situations, which is why people should consider having one.
“We know people struggle to remember important details about their own medical history, including what medicines they have been prescribed or when they received medical treatment – My Health Record can do this for you. By ensuring your medical history is up-to-date and shareable with your healthcare providers, it can help reduce adverse drug events and unnecessary hospital admissions.”
My Health Record is an online summary of a person’s key health information.
It allows them to share and control their health information with doctors, hospitals and other healthcare providers from anywhere, at any time.
The CEO of Winnunga Nimmityjah Aboriginal Health and Community Services in Canberra, Julie Tongs, has seen a significant rise in her clients’ use of My Health Record and is calling on more Indigenous people to also consider the benefits.
Winnunga has more than 7000 clients, many with multiple chronic conditions.
It was an early adopter of My Health Record and now has more than 2430 clients registered.
“For all Aboriginal people this is a great initiative. I will be encouraging our clients to stay with My Health Record,” Ms Tongs said.

“We have 790 transient clients so if, for example, a client from the Northern Territory visits us, it is not easy to get hold of their doctor. Having a My Health Record means our GP can access their important information quickly.
“What’s really exciting now is that more and more information is being uploaded into records. The more information you have, particularly medicines information, the more useful My Health Record is.
“Maintaining privacy is paramount and I am glad that concerns about privacy have been addressed. So my advice now is to jump on board and support it. At the end of the day it will be worth it.”
Australians are being encouraged to create their own My Health Record and test it out during the extended opt out period which now ends on November 15.
Rural and regional Australians stand to benefit the most from having a My Health Record as they have higher exposure to health risks and injury, experience higher levels of disease and have less access to health services compared to people in metropolitan areas.
“Having a My Health Record can be a real life saver for people in the bush who don’t always have easy access to healthcare services,” CEO of the the National Rural Health Alliance Mr Diamond said.
It can save lives in emergency situations, which is why people should consider having one
- Professor Meredith Makeham
“My Health Record offers compelling health benefits, especially for people living in rural and remote areas so it makes sense for people to at least try it before deciding if it is right for them.
“Australians living in rural and remote areas are more likely to end up in an emergency department from a heart attack, car accident or diabetic coma. If they’re unconscious, and the medical team doesn’t have access to their health history, the team may not be able to provide life-saving care.
“If people have hesitations, they should at least test My Health Record themselves during the extended opt out window period as they can always cancel it by 15 November if they’re still not convinced of the benefits.”
According to the National Rural Health Alliance, people living in remote areas are 25 per cent more likely to suffer from coronary heart disease.
They are 40 per cent more likely to die from diabetes, and they are five times as likely to die from a road accident.
People living in remote and very remote areas generally have poorer access to health services than people in regional areas and major cities.
They also have lower rates of bowel cancer screening, higher rates of potentially avoidable hospital admissions, and lower access to selected hospital procedures.
Ian Gillies is a farmer at Yankalilla, south of Adelaide, who served in the Royal New Zealand Air Force.
A regular user of My Health Record, having been in and out of hospital, he compares My Health Record with his time in the aviation industry where all planes had a maintenance log to ensure they operated safely.
“Record keeping has been in the aviation industry ever since it started – every plane has its own maintenance log with it and it is a perfect system,” Mr Gillies said.
“When my Doctor told me about My Health Record, he didn’t have to sell me at all. It provides an opportunity for both myself and my Doctors to have my health issues, treatment and medicines in the one place.
“Like aircraft maintenance data, My Health Record gives you and your healthcare providers the power to immediately investigate what’s happening and what may need special attention.”
By the end of 2018, a My Health Record will be created for every Australian, unless they choose not to have one.
If people choose not to have a My Health Record, they will be able to opt out of having one created for them before November 15, 2018.
More than six million Australians already have a My Health Record and 13,150 healthcare professional organisations are connected, including general practices, hospitals, pharmacies, diagnostic imaging and pathology practices.
The My Health Record is already making healthcare management for individuals and healthcare providers easier and safer, and could save lives in an emergency situation.
More information on My Health Record can be found at www.myhealthrecord.gov.au.

